Our health is being held hostage by high drug prices.
We’ve all heard stories of people who’ve died because they can’t afford life-saving medication—stories like that of Cole Schmidtknecht, who couldn’t afford his asthma inhaler.
Despite advancements in drug manufacturing, drug prices go up—and up, and up.
President Trump highlighted how complex and convoluted the drug pricing scheme is in his first term, and recently signed an executive order that seeks to lower drug prices. With this executive order, President Trump has opened up a world of information about how the health care system delivers prescription drugs and what, exactly, is driving up prescription drug prices.
Some of the major players involved in drug pricing are Pharmacy Benefit Managers, or PBMs.
PBMs are third party middlemen who negotiate prescription drug prices with pharmaceutical manufacturers on behalf of insurance companies, health plans, or government entities. PBMs have incredible influence on who gets what medication, and at what cost.
PBMs control which drugs are available on your health plan. If the drug isn’t on the list, your insurance company won’t cover it. To make sure their drugs are included on the list, drug manufacturers will give a “rebate” to the PBM, a portion of which the PBM keeps. This kickback goes directly into the pocket of both PBM’s and insurers. Oftentimes, the higher the drug price, the bigger the kickback.
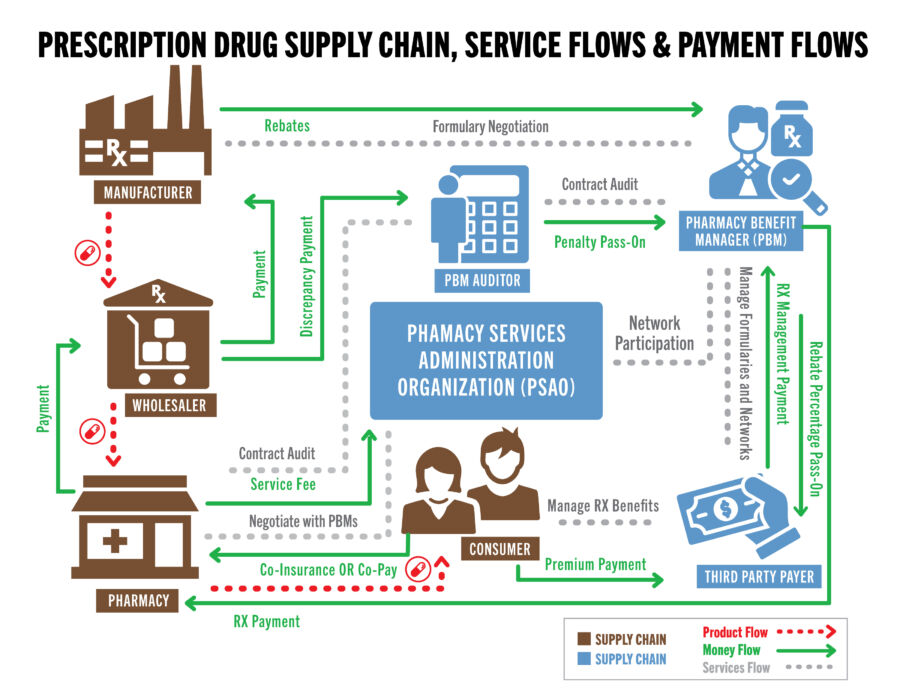
PBMs are just one player that operates in the drug pricing ecosystem in the U.S. There are at least four—and sometimes more—different groups that are making money when a patient picks up their prescription from the pharmacy. Some key players are:
- The pharmacy and pharmacist
- The PBM
- The drug wholesaler
- The insurance company (via premiums)
It’s a complex system that we’ve illustrated with the chart below:
But PBMs aren’t just middlemen and negotiators—they have been accused of engaging in monopolistic behavior and some are being investigated by the Federal Trade Commission right now.
However, the problems don’t start or stop with PBMs—America’s drug manufacturing complex is also in serious need of rework. Right now, over 90% of drug precursors come from China, which has significantly lower quality control. Additionally, there’s the obvious national security risk: in the event of a supply chain disruption, hundreds of thousands of Texans would have their medicines run out.
However, there are a couple things that Texas can do to help bring down the price of drugs. First, they could allow—like 46 other states—direct dispensing of prescription drugs by physicians. This would remove PBMs, insurance, and pharmacists from the drug pricing equation, bypass prior authorization restrictions, and re-establish a close relationship between doctors and patients.
Second, Texas needs to make serious moves towards promoting domestic drug manufacturing. Utah looked at this with a “States Cures Compact,” which would pool resources together from neighboring states to develop cures for common diseases and then turn the intellectual property over to the public.
Texas could build on this idea by forming a “manufacturing quota” compact where drugmakers could bid for the right to produce high-demand medications at scale, thus increasing supply and lowering prices.
Finally, Texas needs to push for more transparency in the prescription drug market. Texans are not aware that the drugs they are purchasing are filled with contaminated or possess toxic substances. Requiring a “truth in origin” label could alter Texans’ purchasing behavior and obtain better quality drugs made in America.
Texas can bring down drug prices without engaging in price controls—and it’s time for Texas to take strong steps towards doing so now.
Lives depend on it.